
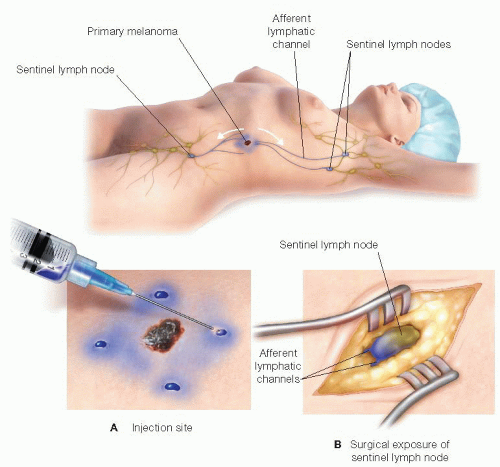
Its impact on the overall cost of melanoma care is intimately tied to systemic therapy in the adjuvant and recurrent settings.Ĭost-effectiveness Melanoma Sentinel node biopsy. The sentinel lymph node (SLN) is defined as the lymph node (LN) that receives drainage from the tumour. However, a treatment plan that forgoes adjuvant therapy for resected stage IIIA melanoma but offers systemic therapy for a node-basin recurrence would nullify the additional cost of SLNB. Estimates for 5-year costs reflect a fourfold increase in total costs of care associated with SLNB. Ulceration (HR 4.7, p = 0.022) and positive sentinel node (HR 11.5, p < 0.001) were associated with worse MSS. Patients who underwent SLNB had higher 10-year nodal recurrence-free survival (98.6% vs. If the cancer has spread to a lymph node, you have. If cancer is found in a sentinel lymph node, a surgeon may need to remove the remaining lymph nodes. Having a sentinel lymph node biopsy (SLNB) can tell whether cancer cells have spread to a nearby lymph node. However, not all patients with melanoma require a sentinel lymph node biopsy. For melanoma, the basics of the procedure are the same. If a lumpectomy is also being performed, an extra 30-45 minutes are usually added to the total surgery time. Helps doctors make a prognosis and develop an individualized treatment plan based on the extent of the spread of cancer. A sentinel node biopsy typically takes about 45 minutes to perform. A Markov model was created to estimate long-term costs.Īmong the total 392 patients, 238 underwent SLNB. A procedure to determine whether cancer has spread to the lymph nodes. Institutional costs of melanoma care were converted to Medicare proportional dollars.

Results of SLNB, completion lymphadenectomy (CLND), recurrence, and melanoma-specific survival (MSS) were assessed. See " New Guideline Limits Need for Extensive Lymph Node Removal for Breast Cancer.The purpose of this study is to report the additional prognostic information and cost associated with sentinel lymph node biopsy (SLNB) for patients with T1b melanoma.Īn institutional database was queried for patients with T1b melanoma (0.8-1.0 mm or < 0.8 mm with ulceration) with at least 5 years of follow-up. Learn more about the sentinel lymph node biopsy procedure.
#Sentinel node full#
"It has been shown to be a safe and accurate alternative to full axillary surgery in patients with breast cancer, and constitutes an important advance in breast cancer surgery." Sentinel nodes are the first lymph nodes where cancer cells might spread from a tumor. During this procedure, the healthcare provider removes the sentinel nodes and sends them to a lab to test for cancer cells. Baldwin Breast Care Center, says, "Sentinel node biopsy is now standard treatment. A sentinel node biopsy (also called a sentinel lymph node biopsy or SLNB) is a surgical procedure for people with cancer. O'Hea, MD, associate professor of surgery and chief of breast surgery, and medical director of Stony Brook's Carol M. An incision is then made in that location, and the sentinel node, identified by both the gamma probe and the blue dye, is removed.Īn early proponent of sentinel node biopsy, Brian J. Next, the surgeon uses a geiger counter-like device (probe) to locate and count the small amount of radioactivity injected earlier, which is now trapped in the first draining axillary lymph node (sentinel node). Both the blue dye and the radioactive dye travel towards the patient's underarm via lymph vessels, helping the surgeon to find that first draining lymph node. In the operating room, a small amount of blue dye is injected around the tumor as well. These are also the first lymph nodes where breast cancer is likely. The amount of radioactivity is very small, less than that used for a chest x-ray or a bone scan, and generally does not cause any problems. The first axillary lymph nodes to absorb the tracer or dye are called the sentinel nodes. This test helps to determine the location of the lymph nodes that are draining the breast cancer. In sentinel node biopsy, a small amount of radioactive dye is injected into the breast around the site of the cancer. A lymphoscintigraphy, or sentinel lymph node scan, is a test used to find which lymph nodes are the first to get fluid drainage from the area of the body.


 0 kommentar(er)
0 kommentar(er)
